is my full-time job to make health care easier for Utah’s newcomers using the Redwood Health Center. On a daily basis, I help newcomers solve problems with their case workers and interpreters, coordinate with resettlement and migration agencies, support our clinicians, and teach staff how to create an inclusive and more patient-centered experience for patients.
Over the last five years, I’ve learned a lot about our new American patients who were once forced to flee their home countries. When they walk through our clinic doors, they are in new surroundings, and are vulnerable in ways that other patients are not. They may have tremendous care coordination challenges. The path to better care for newcomers starts with better coordination between care teams, resettlement and migration agencies, community partners, and the new American community. Better coordination helps not only our newcomers, but all of our patients.
Here are three suggestions to help make caring for newcomers easier.
Tip #1: Utilize the New American Form and Identifier
U of U Health New American Resources
The New American Resource page on Pulse has a wealth of useful information.
Here’s a link to the tip sheet for utilizing the 'New American Form and Identifier' in Epic.
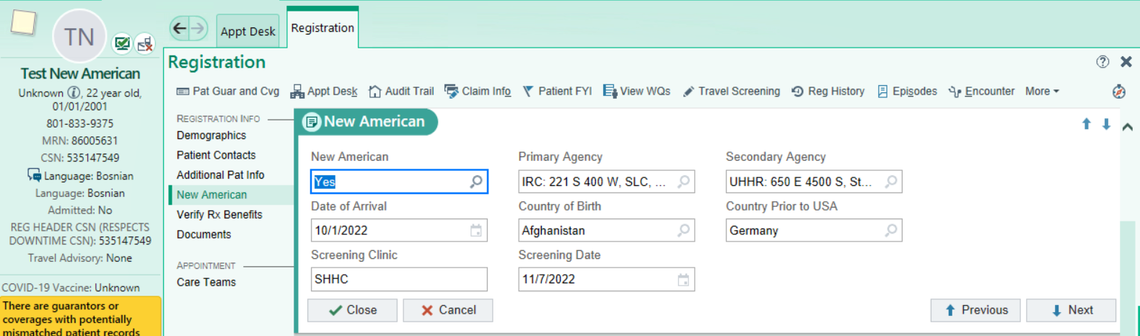
I helped create a tool in Epic that helps care teams working with patients of refugee background by providing essential care information in a single location. Formerly known as the FYI Flag, the New American Form stores resettlement information, for both newly arrived and previously resettled patients, so that appropriate care teams within the U Health system will be alerted and can offer culturally responsive care. The form prompts the entering user to collect key information: the agency that is providing case management and coordination for the patient, a secondary agency providing coordination and support (if applicable), the patient’s date of arrival to the United States, their country of origin, the country they resided in prior to coming to the United States (if applicable), their domestic initial health screening clinic, and date of the health screening.
Screen grab of New American Resettlement Information Form in Epic, Coming April 16th, 2023 with the Epic Upgrade:
Demographics Collection View:
Collection and utilization of resettlement information is important for three reasons. First, it allows U Health to close care gaps and improve health equity on both an individual level and a system level. We can zoom into a marginalized patient population and approach culturally responsive outreach, modified practices, and view health outcomes. Second, the identifier provides an important cultural cue to the care team, signaling them to tap into trauma informed care techniques or special protocols based upon the population’s needs. For example, a provider might need to be aware of their patient’s country of origin so they know what priority health conditions as well as trauma to look out for based upon CDC recommendations. Third, the information allows multiple care teams support in contacting resources and finding culturally applicable services for the patient. For example, a patient within a case management period (usually a set date of one year from their date of arrival) has access to specialized resources in comparison to a patient who is out of case management.
Thanks to Truly Ashby in revenue cycle who helped me set up the original FYI Flag in March 2018! And another special thanks for the RAE Committee for helping to reimagine the enhanced collection form!
Tip #2: Plan to spend more time on education and health literacy
Visiting a U Health facility can often be a patient’s first encounter with a Western medicine system. If your patient is having difficulty complying with their care plan, it may be due to health literacy. It is not uncommon for patients, from any background, to have a hard time digesting and complying with advice given by a health care provider. The language and cultural differences between Western care providers and newcomer patients can make compliance complex. You might consider the following practices:
-
Don’t be afraid to ask questions for clarification. Asking questions to verify comprehension is a good way to connect and teach health literacy. It allows you to provide additional context or education where necessary. Consider utilizing the teach back method.
-
Don’t be afraid to use the iPad as the interpreter. We cannot improve health literacy without communicating to the patient in their preferred language. In-person interpreters are not always available and many patients prefer the iPad to having an interpreter there in person. Interpreting Services has 3 applications contracted for medical use: Cyracom, AMN, and Martti. Interpretation is a service we must provide and we should not be using family members or minors.
-
Utilize translated forms, visual, and audio aids. There are often forms that are more culturally appropriate for patients who are not native to the United States. Translation Services and Patient Education teams can help create forms to fulfill your patients’ needs if they don’t already exist. If a patient has a camera phone, they may want to record instructions you give them while the interpreter interprets.
Tip #3: Take a more holistic view of the patient
At the core of caring for new American patients is a willingness to take a holistic view of the patient. Many patients don’t realize, their physical, mental, social, and spiritual wellbeing is all connected. They may not be able to focus on their diabetes until their housing concerns are taken care of. Utilizing all disciplines like social work, care management, pharmacy, and nutrition for the care team will be helpful. Branches of the extended community care team may need to support as well. Don’t forget the resettlement agencies, community based organizations, and community health workers can support different social determinants of health.
New American patients face unique challenges that may seem incomprehensible to many of us. Demonstrating empathy is an important way of connecting with patients and, as research demonstrates, can improve outcomes. Demonstrate empathy by asking about their work, how they're settling in to Utah, educational classes, how they’re adjusting to Utah weather,—not just their physical health.
Think about what it takes for some of these patients to be in clinic. Maybe they had to take two busses. Maybe they struggled to get time off. There are new challenges and systems to navigate. Give them time and take the time to build a connection with them.
Your patients aren’t alone—and neither are you
Clinicians often feel overwhelmed by complex patient needs because there are so many variables out of their control. New American patients may experience cultural and economic barriers that can be hazardous to their health and well-being. There are a host of services available for newcomers and tools available to busy providers. A lot is at stake for these patients and we can provide culturally responsive care by using the available tools (New American Form and Identifier, Interpreting Services), resources (care teams, CDC, agencies), getting to know them as individuals, and treating them holistically. Take advantage of research, webinars, and opportunities to learn more about this population so you may incorporate that knowledge into your patient interactions.
Resources:
Understanding Resettlement and Refugee Health
- Utah Department of Health Refugee Health Program
- Cultural Competency Powerpoint for Health Care Providers by OHEDI and UUHP
- CDC Immigrant and Refugee Health
- Switchboard Resettlement Experts Webinars and Resources
Local Resources for Patients and Care Teams
- The Mayor’s Office for New Americans: Resource center
- The Refugee Center/Refugee Services Office: Resource center
- The International Rescue Committee: Resettlement agency and resource center
- Catholic Community Services: Resettlement agency and resource center
- Asian Association of Utah – Refugee and Immigrant Center: Secondary migration agency and mental health resource
- Utah Health and Human Rights: Mental health resource
- Take Care Utah: Medicaid/Marketplace enrollment assistance
- Utah Immigration Collaborative: Legal services for the community
- University Neighborhood Partners: Hartland resource walk-in Center
Resources for Care Team Self-Care
- Heal Torture: Self-Care for secondary traumatic stress
Teach Back Method
National Level Resources
Rave Reviews for Anna's Work
| "Anna has been instrumental in helping new refugee arrivals better understand and access health care within the United States. She goes over and beyond to help not only support clients, but also does so much to help support the refugee resettlement organizations. Working on projects such as preventative health care and pregnancy classes for refugees has helped our clients to not only have a more holistic approach to healthcare, but also to feel valued." |
— Jenny Hart, Maternal & Child Health Program Coordinator, International Rescue Committee
| Anna facilitates a class taught by Dr. Keri Gibson for pregnant refugee women at Redwood on the second Tuesday of every month. "One of the challenges and unique opportunities of this class is the combination of different cultures. The languages range from three to seven per class. Currently, they have three iPads and 3-4 interpreters attending to translate for our patients in this session...They reorganize the conference room for each class to create a more inviting atmosphere, have all female staff, interpreters, and volunteers, which is more adaptable to their learning and comfortable for them to interact. Anna has been working closely with the agencies and the OB team to get things coordinated and a process in place. This is such a great example of overcoming barriers, adapting, and really going that extra step to provide the care and education that these patients need, in a safe environment." |
— Nickole Canfield, Administrative Office Specialist at Redwood Health Center
This article was originally published August 22, 2019.
Anna Gallegos
U of U Health recently received the LGBTQ Health Care Equality Top Performer designation from the Human Rights Campaign Foundation—but this achievement didn’t happen overnight. Plastic surgeon and Transgender Health Program Director Cori Agarwal, and Program Coordinator Ariel Malan, share the grit, determination and patient collaboration that transformed our health care system.
Transgender and gender diverse patients face systemic discrimination in our broader society and inequitable access to needed care. Ariel Malan, program coordinator and Andy Rivera, volunteer for Utah’s Transgender Health Program, share how to create an inclusive care environment for this vulnerable population focused on trust and respect.
The crises of Covid-19 and police brutality have highlighted systemic racial inequity in the United States and the need to consciously dismantle the forces that cause racial health disparities. PA students Scarlett Reyes and Jocelyn Cortez brought together Black patients at the University of Utah to share their experiences. Their advice: build cultural competence and be mindful of microaggressions.
