Objectives
1) Convey respect by utilizing appropriate LGBTQ+ terminology
2) Identify best practices for interacting with transgender and gender diverse patients
3) Implement strategies for fostering cross-cultural care
ransgender and gender diverse people are one of the most at-risk populations in the United States. Trans people earn less, are less likely to be in jobs with health care coverage, and face significant socioeconomic barriers in housing, education, and mental health.1 All of these issues are even more prevalent for trans people of color.2 Because of these adverse social determinants of health, trans people are more likely to suffer from serious health conditions. Researchers have also found that trans people often delay or avoid routine care because of fear of discrimination from the clinical team.3
It’s important that we deliberately build trust with transgender and gender diverse patients to combat discrimination and to support improvement of their health outcomes, both for routine care and for interventions like hormone therapy and surgery. By learning the appropriate terminology and simple strategies for better communication, we can demonstrate respect and inclusivity.
Who is the LGBTQ+ population?
Our patients are placing their trust in us. By investing our time in grasping basic terminology and understanding sexuality, gender identity, and gender expression, we can promote a safe, affirming environment for all patients.
Transgender Health Program
Utah’s Transgender Health Program strives to provide comprehensive, compassionate, gender-affirming care for our transgender and gender diverse patients. Since its inception in 2017, the program has tripled in volume to meet community demand for these services. Today, our multidisciplinary services span over eight specialties and 40 providers.
Know the terminology
Quality of care relies heavily on open communication by both patients and providers. Let’s establish a basic understanding of the common LGBTQ+ terminology.
Refers to women who are attracted to women.
Refers to men who are attracted to men.
Refers to an individual who is attracted to both genders.
Refers to an individual who is attracted to people, regardless of gender.
Refers to an individual who doesn't necessarily identify with the gender they were born with, which is often decided by an individual's sex assigned at birth.
Although once used as a slur, queer has been reclaimed by the LGBTQ+ community as an umbrella term that may describe an individual’s gender identity, sexual orientation or both.
Try not to think of these terms as labels you would apply to someone, but more as some of the ways that patients will self-identify.
Just as health care constantly evolves, so too does terminology. Understand that as people reclaim identities, terms may change. View and download a pdf of updated terminology here.
Understand sexuality, gender identity, and gender expression
While these three terms are frequently confused, the distinctions between them are very important.
Sexuality refers to an individual’s personal attractions, or who they’re attracted to romantically or sexually.
Gender Identity is a person’s internal sense of their gender. Do they consider themselves male or female, neither or both? Being cognizant of how an individual defines their gender identity and the terminology that they prefer is an act of respect. Some of the acronyms and terms that you might see include:
-
FTM (female to male)/transgender male/trans masculine: An individual who was assigned female at birth but identifies as male.
-
MTF (male to female)/transgender female/trans feminine: An individual who was assigned male at birth but identifies as female.
-
GNC (gender non-conforming): An individual who doesn’t necessarily identify as exclusively male or female. They may see their gender identity on a spectrum, or as androgynous (somewhere in the middle).
-
GQ (gender queer): An umbrella term that describes a person whose gender identity falls outside the traditional gender binary of male and female. Some people use the term gender expansive.
-
NB (non-binary): An individual whose gender identity falls outside of the traditional gender binary structure of girl/woman and boy/man.
-
Agender: An individual who identifies as having no gender, or who does not experience gender as a primary identity component.
-
Questioning: An individual who is questioning their sexuality and gender identity. This person might identify with the LGBTQ+ community but still doesn't know where they fit within that spectrum.
-
Intersex: Describes a group of congenital conditions in which the reproductive organs, genitals, and/or other sexual anatomy do not develop according to traditional expectations for females or males. Intersex can also be used as an identity term for someone with one of these conditions. The medical community sometimes uses the term “differences of sex development” (DSD) to describe intersex conditions; however, the term intersex is recommended by several intersex community members and groups.
Gender Expression is how a person externally presents and expresses their gender through their behavior, mannerisms, speech patterns, and dress. Gender expression, like gender identity, often falls on a spectrum.
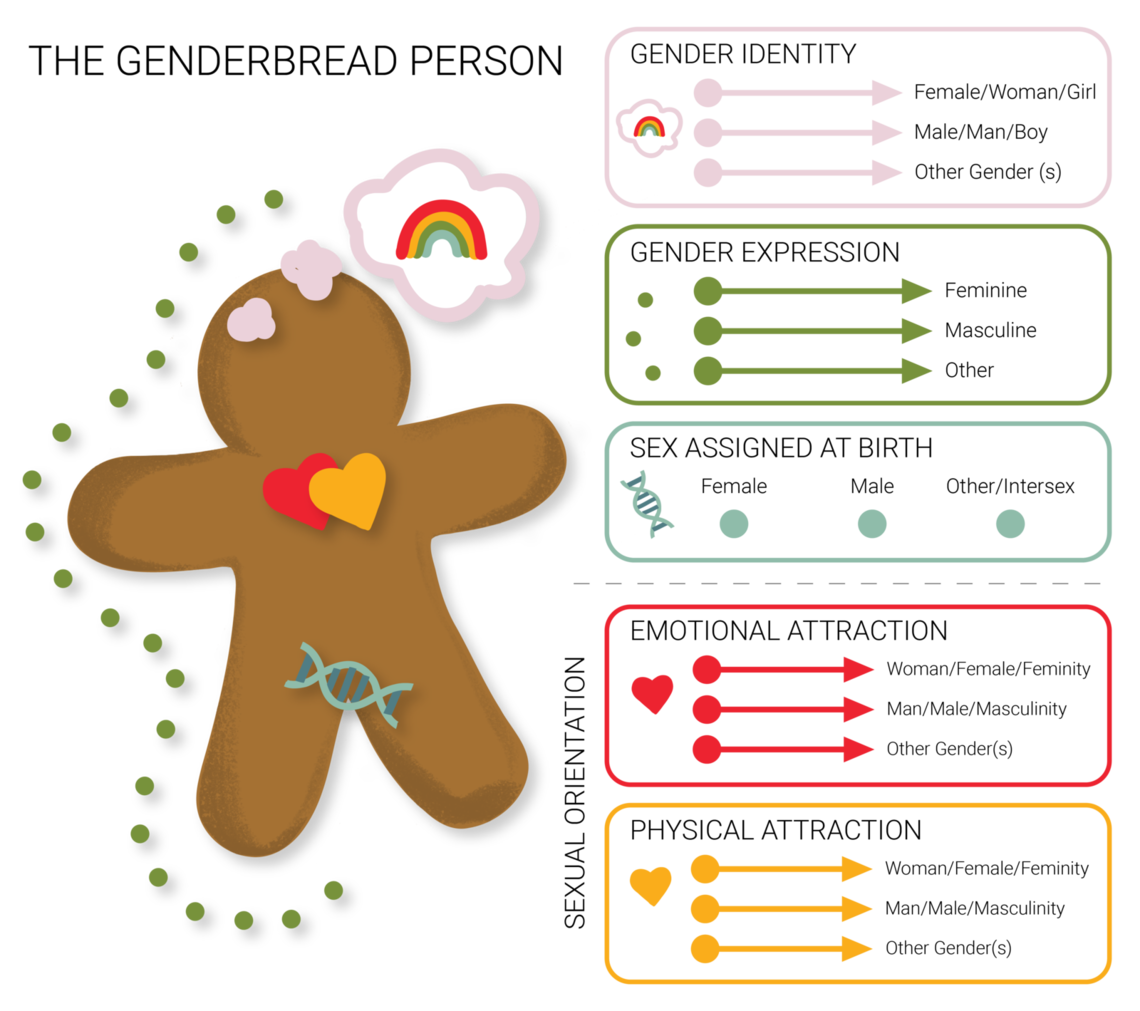
In order to differentiate between sexuality, gender identity, gender expression and biological sex, let’s take a look at the Genderbread Person below.
Note that individuals’ gender identity or expression do not indicate their sexual orientation or sex assigned at birth and vice versa.
What you can do: Best practices for exceptional care
#1: Embrace cross-cultural care
Cross-cultural care focuses on the ability to communicate effectively with patients from diverse backgrounds. These three principles of cross-cultural care can help you create a safe space for your patient:
-
Respect: Live by the golden rule and treat your patients as you’d want to be treated.
-
Curiosity: It’s okay to be curious; we’re only human. Before you ask a question, put yourself in the patient’s shoes, and appreciate that they’re likely feeling vulnerable and apprehensive. Make sure your questions are medically relevant and respectful.
-
Empathy: Establish rapport with your patients by asking appropriate questions, and encouraging open discussion based on mutual trust.
#2: Ask for pronouns and document appropriately in Epic
While we often don’t think twice about assuming people’s pronouns based on physical appearance, it’s important to recognize that pronouns don’t always parallel an individual’s appearance or gender identity. Misgendering, or using someone’s incorrect pronouns can be harmful even if unintentional. We can all recognize the conventional pronouns, but when it comes to gender-neutral pronouns like “they/them/theirs,” and “ze/zir/zirs,” many of us are still in the dark.
Pronoun Resources
Pronoun Guide — from Utah's Transgender Health Program
Gender Pronouns Table — from Trans Student Educational Resources
Although it might seem counter-intuitive to use “they/them/theirs” as a pronoun for an individual, it’s actually a good, safe gender-neutral pronoun. In the event that somebody provides you with pronouns that you're not familiar with, it’s okay to ask them things like "How do you spell it? How do you pronounce it? What is the best way to use it in subjective and objective as well as possessive and reflexive?" As important as it is to ask a person's pronouns, it's equally important to use the pronouns they give you. It’s also ok to make a mistake. If you do, apologize, correct yourself and move on.
One of the biggest ways we can respect and support our transgender and gender diverse patients is by documenting their chosen names and pronouns in Epic. Many times, these individuals’ legal identification doesn’t align with how they self-identify. By documenting their information appropriately, you’re respecting their identity and setting a precedent on how our clinics should treat all patients.
#3: Create a welcoming environment
Simple gestures, like signs of affirmation and acceptance (a pronoun pin on your badge, a rainbow sticker, etc.) or magazines and pamphlets that represent the patient population go a long way. Think about the details, like the paperwork you hand out. Design paperwork that is inclusive, not exclusive, by including space for chosen names, sexual orientation and gender identity.
#4: Know where to refer a patient for more resources
The gender journey of every patient is unique. Although some people who identify as transgender or gender diverse desire to medically transition, not all do. It’s important as health care providers to not assume what someone’s journey might look like but to be aware of the services offered to patients.
We’re here to help—contact the U of U Health Transgender Health Program.
#5: Expand you and your staff’s competency
Sharing resources, like this article, and continuously building skills is an investment in your staff.
Remember that you don’t have to be an LGBTQ+ health care expert—you don’t have to read every book or attend every training session. Here are some basic tips to improve communication with patients:
| Be aware of this | Try this instead | |
|---|---|---|
| All patients do not use traditional labels. | Follow the patient’s lead in discussing sexuality and gender identity. | |
| Don’t assume orientation or identity based on appearance, partner(s), or behaviors. | When in doubt, ask. | |
| Don’t assume a patient’s orientation based on gender. |
|
|
| Avoid stereotypes or asking questions that are not necessary for care. | Frame questions in a respectful manner. |
Resources
Request this training for your department here.
-
SOGI Pulse Page includes tips sheets and more
-
Patient Voices seminar: Transgender and Gender Diverse Patient Experiences in Health Care
-
World Professional Association for Transgender Health (WPATH)
References
-
Barriers to Health Care for Transgender Individuals. Safer JD, et al. Curr Opin Endocrinol Diabetes Obes. 2016 Apr 1; 23(2):168-171.
-
Report of the U.S. Transgender Survey 2015. National Center for Transgender Equality.
-
Transgender noninclusive healthcare and delaying care because of fear: Connections to general health and mental health among transgender adults. Seelman KL, et al. Transgender Health. 2017 Feb 1;2(1):17-28.
Originally posted October 2020
Ariel Malan
Andy Rivera
The crises of Covid-19 and police brutality have highlighted systemic racial inequity in the United States and the need to consciously dismantle the forces that cause racial health disparities. PA students Scarlett Reyes and Jocelyn Cortez brought together Black patients at the University of Utah to share their experiences. Their advice: build cultural competence and be mindful of microaggressions.
U of U Health recently received the LGBTQ Health Care Equality Top Performer designation from the Human Rights Campaign Foundation—but this achievement didn’t happen overnight. Plastic surgeon and Transgender Health Program Director Cori Agarwal, and Program Coordinator Ariel Malan, share the grit, determination and patient collaboration that transformed our health care system.
As Redwood Health Center’s program coordinator serving new Americans, Anna Gallegos has learned valuable lessons that can help all of us better care for patients of refugee background and vulnerable populations. Here are three suggestions to help make caring for patients easier.
