eginning in June 2023 and after 2 years’ of preparation, University of Utah Health is expanding its list of racial and ethnic identities. This new list will be available to patients to self-select as they complete demographic information during registration. We hope this change will create better visibility for all identities, enable effective inclusive care, and improve equity of health outcomes.
Front desk and scheduling team members will ask patients to choose from an expanded list, either in-person or on the phone. Patients may also complete this information via myChart.
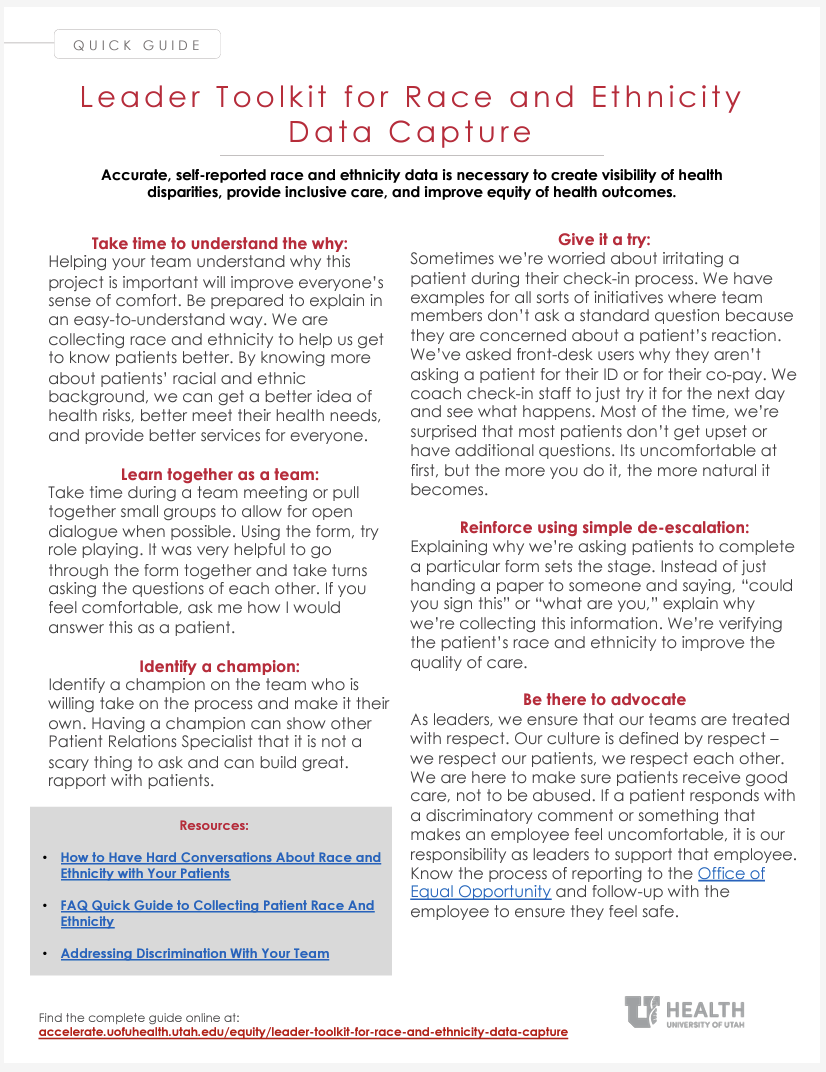
Leaders may be wondering how to best prepare their teams. Below are “lessons learned” after conducting a pilot with 5 locations, over 300 patients and 30 team members.
We learned from the pilot that we needed to focus on small-group discussions with teams focused on conversation and learning together. Exploring the purpose of the project and practicing together built confidence in holding potentially uncomfortable conversations with patients. We also found many team members and patients excited to better represent their identity through more options and the ability to choose more than one.
We’ll continue to refine our training program as the process is implemented and we learn from our findings.
Start with why. Helping your team understand why this project is important will improve everyone’s sense of comfort.
Be prepared to explain in an easy-to-understand way:
- We are collecting race and ethnicity to help us get to know patients better.
- Knowing more about patients’ racial and ethnic background gives us a better idea of health risks, so we can better meet their health needs, and provide better services for everyone.
Read the article: More Than 'Some Other Race'... (4 minutes)
Take time during a team meeting or pull together small groups to allow for open dialogue when possible. Using the form, try role playing. It was very helpful to go through the form together and take turns asking the questions of each other.
One team who participated in the pilot didn’t get a chance to spend time together learning about the race and ethnicity pilot, and it showed. The team wasn’t comfortable with gathering the information. It showed us how important it was to have an opportunity to role-play and discuss in person.
Read the article: "How to Have Hard Conversations..." (3 minutes)
What it looks like in practice:
When I (Erica) did a session for the care navigation team, I asked questions to allow for open conversation. One of our team spoke up to say that they were proud that the U was doing this project, and how they had been waiting for this. That really lifted everyone's spirits.
At Redwood, I (Theresa) led the team’s conversation in staff meeting. We thought, what better way to break down discomfort than to invite people to talk about their hesitations? The open dialogue led to some role playing. A lot of them really enjoyed being angry patients! But having that opportunity to answer each other’s questions and especially the harder escalated questions made it a lot easier once it was time to do it in real life.
We (at Redwood) had a champion on our team, Nicole Misner, who just took the process and made it her own. She wasn’t afraid and became really confident. Having a champion showed the other Patient Relations Specialist that it wasn't really a scary thing to ask. When I shadowed Nicole, I saw how she had made the race and ethnicity question a part of her flow. She has great rapport with patients.
Read the article: "How to Have Hard Conversations About Race and Ethnicity With Patients..." (3 minutes)
Sometimes we’re worried about irritating a patient during their check-in process. We have examples for all sorts of initiatives where team members don’t ask a standard question because they are concerned about a patient’s reaction. We’ve asked front-desk users why they aren’t asking a patient for their ID or for their co-pay. We coach check-in staff to just try it for the next day and see what happens. Most of the time, we’re surprised that most patients don’t get upset or have additional questions. Its uncomfortable at first, but the more you do it, the more natural it becomes.
Its easy to think about the negative things that could come when you ask about race and ethnicity, but we also encountered positive reactions. I (Theresa) am biracial and I always felt like I had to pick. When I started working on this project, I went into myChart and saw that at some point, someone had picked a race and ethnicity for me and my children. I changed the fields in myChart, and it felt like being seen. We can all be seen - we can all choose to represent all of our different cultures.
Read the article: "Why It Shouldn't Be So Hard..." (3 minutes) Our colleagues at the Zero Suicide program partner with a U of U researcher to make asking hard questions easier.
Explaining why we’re asking patients to complete a particular form sets the stage. Instead of just handing a paper to someone and saying “could you sign this” or “what are you,” explain why we’re collecting this information. Here it is: we’re verifying the patient’s race and ethnicity to improve the quality of care.
Help the team use the FAQs when a patient asks a question. When team members respond with “I have to ask you as part of my job,” it demonstrates a lack of confidence to the patient and erodes trust in the health care team. Patients will mirror our attitude and behaviors.
Take cues from the patient. If the patient is uncomfortable, its ok to mark “choose not to disclose.” Be ready with a respectful response: “That’s ok, I’m going to go ahead and select choose not to share.” We’re not asking anyone to battle with patients, and ultimately we want everyone to feel respected.
Read the FAQ: Frequently Asked Questions About Collecting Patient Race and Ethnicity (3 minutes)
As leaders, we ensure that our teams are treated with respect. Our culture is defined by respect—we respect our patients, we respect each other. We are here to make sure patients receive good care, not to be abused. If a patient responds with a discriminatory comment or something that makes an employee feel uncomfortable, it is our responsibility as leaders to support that employee. Know the process of reporting to the Office of Equal Opportunity and follow-up with the employee to ensure they feel safe.
As a person of color, when I (Theresa) ask the question, that's one of the first things I think about—am I going to offend somebody? Are they going to respond unkindly? When I was a Patient Relations Specialist, I had a really supportive manager and supervisor who would pull me aside side and just say, "Hey, sometimes you're not going to have a really nice patient but don't take it personally. Its not ok and we can talk to that patient about their behavior.” If your leader is there to support you and let you know that they're there for you, it makes a difference.
Read the article: Addressing Discrimination With Your Team (4 minutes)
Kim Birrell
Theresa Johnson
Erica Ulibarri
Accurate, self-reported race and ethnicity data is necessary to create visibility of health disparities, provide inclusive care, and improve equity of health outcomes. Redwood Health Center’s Patient Relations Specialist Nichole Misner shares how to respectfully discuss this needed health information with patients.
Accurate, self-reported race and ethnicity data is necessary to create visibility of health disparities, provide inclusive care, and improve equity of health outcomes. Community engagement director RyLee Curtis, Chief Quality Officer Sandi Gulbransen, Project Manager Kimberly Killam, Patient Experience Director Mari Ransco, Chief Medical Informatics Officer Michael Strong, and Health Sciences Equity, Diversity, and Inclusion Librarian Donna Baluchi explain how University of Utah is improving data quality.
Huntsman radiation oncologist and population health scientist Gita Suneja, and maternal-fetal medicine specialist and racial, ethnic, and geographic disparities researcher Micelle Debbink, share five practical steps health sciences educators, researchers, and clinicians can take toward delivering more equitable care today.