‘CHOOSE FROM THE OPTIONS BELOW.’
Patient voice: “This seemingly innocuous prompt embedded in countless daily medical registrations aims to capture race and ethnicity. Yet, as mothers of children with multiple racial and ethnic identities, a prompt that could take just moments sometimes becomes a weighted pause, reminding us of the intersectional reality of our families.
How do we represent the Thai and non-Hispanic White; Cuban and Vietnamese; Colombian, non-Hispanic Black, and non-Hispanic White backgrounds, roots, and cultures that our children embody? Which box or boxes do we check off?”
From: The Complicated Inadequacy of Race and Ethnicity Data (JAMA Pediatrics 2022)
itting racial and ethnic identity into a tidy box is nearly impossible. Many of us view our heritage in complex ways. In the 2020 US Census, “some other race” was selected by 49.9 million people, making it the second most common racial category. Yet, a large grouping of “other” or “unknown” backgrounds translate to a dead-end for health care improvement. To provide effective patient-centered care for our community, we must have better data. Reliable data—especially racial, ethnic, linguistic, sexual orientation, and gender identity data—is necessary to reduce and ultimately eliminate disparities in health care.
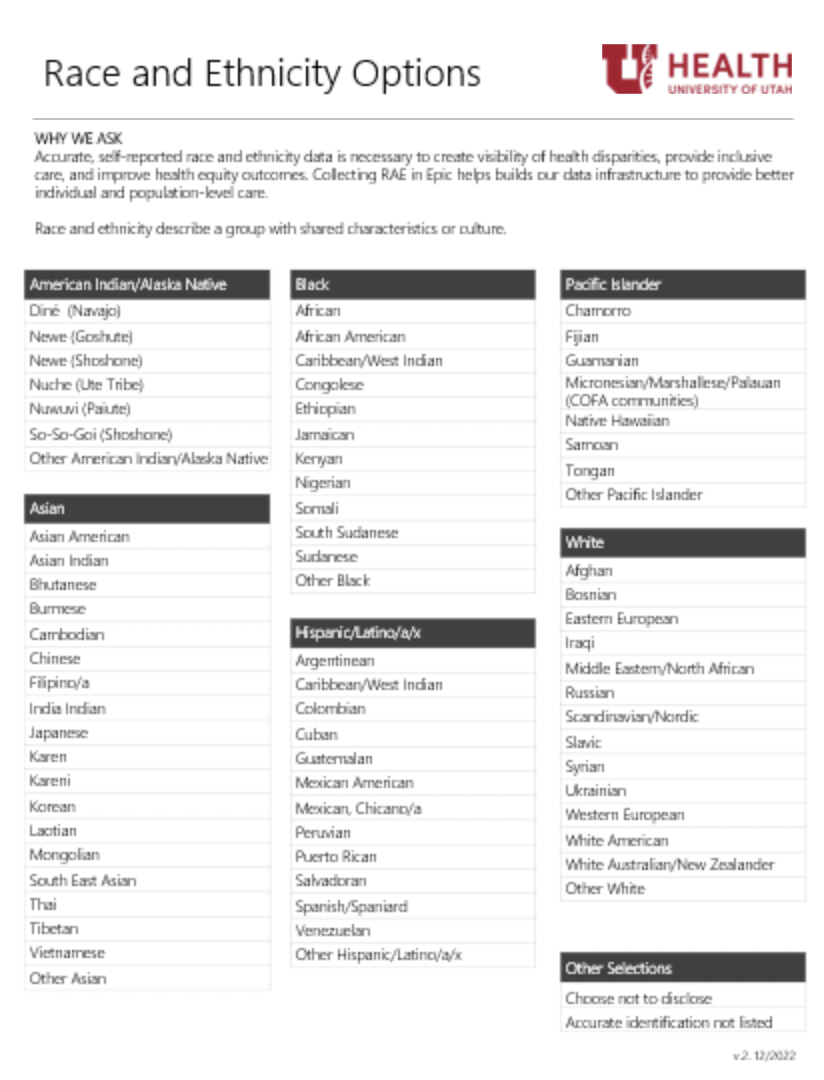
Beginning in June 2023 and after 2 years of preparation, University of Utah Health is expanding its list of racial and ethnic identities. This new list will be available to patients to self-select as they complete demographic information during registration.
We hope this change will create better visibility for all identities, enable effective inclusive care, and improve equity of health outcomes.
The problem of “other”/”unknown”
Currently over a quarter of Unviersity of Utah’s patient population is listed as “unknown” or “other” racial and ethnic identity. We had to ask ourselves—why? Utah isn’t alone in this gap. Inaccurate or incomplete racial and ethnic data in health care is a national problem.
Researchers in 2019 explored why racial and ethnic data remains incomplete, after more than a decade of mandatory collection required by CMS. They found that racial and ethnic identity was often observed, not asked, of patients to self-report. There was cultural insensitivity and a lack of understanding around how to ask. Importantly, many people didn’t see themselves in the eight to ten options provided to them.
Both national and local groups have called for action to improve racial and ethnic data in health care. Groups such as the National Institutes of Health, the American Hospital Association, the Institute for Healthcare Improvement, the Association of Academic Medical Centers, and locally, the Utah Hospital Association and the State of Utah have called for improvements to data quality to improve access to affordable, equitable care.
These same trends are at work here in Utah. University of Utah’s Kem C. Gardner Policy Institute projects that Utah will continue to diversify. The underrepresented populations are projected to increase from the current 20% to 35% in 2065, with faster growth amongst those identifying as one or more race or ethnicity.
We need to understand our patients’ backgrounds to design effective interventions in partnership with communities. For example, we saw that patients who identified as “unknown” were 11% less likely to receive their first Covid vaccine. Without being able to explore the barriers, we were unable to design appropriate interventions. Culturally appropriate care will improve the health of our community, save lives, and reduce health care costs.
Designing with community
Because there is no standardized national race and ethnicity list for University of Utah to implement, we partnered with groups across our system to develop a more inclusive list. We partnered with refugee service organizations to identify the top countries of origin for new Americans in Utah. The Urban Indian Center of Salt Lake guided us to the names of indigenous groups in their respective language, and included the colonized versions second (e.g. Diné/Navajo).
Our list was in the final draft when the State of Utah released their updated guidelines and draft list. We’ve learned through partnership and consultation with them and our surrounding states’ Departments of Health, including Nevada, Idaho, Wyoming, and Colorado.
The diverse University of Utah community has supported this work by bringing their own perspectives and constituencies to inform the project. They are:
- Abdulkhaliq Barbaar, Director, Health Equity, Diversity, and Inclusion
- Kim Birrell, Manager, Patient Access
- Anna Gallegos, Program Coordinator, Redwood Health Center New American Support
- Travis Gregory, Senior Director, Information Technology Systems
- Marcie Hopkins, Manager, Human-Centered Design, Patient Experience & Accelerate
- Theresa Johnson, Revenue Cycle Coordinator
- Kim Pacheco, Director, Revenue Cycle Support Services and Patient Access
- Terrel Rohm, Director, System Quality Analytics & Technology
- Erica Ulibarri, Program Coordinator, Care Navigation
- Mikayla Schaefer, Director, Project Management
Partners in Information Technology Services, Enterprise Data Warehouse, and Decision Support have made this project a reality. Amy Sneddon, Wade Bourland, John Colt, Vicki Wells, Christy Benson, Ming Tu, Reed Barney, and Candice Crawford designed the technical solutions, outward-facing solutions for patients and back-end mapping to enable reporting.
Testing the process
Our literature review and research with other organizations revealed a needed focus on both the knowledge and comfort of front-desk personnel who would be discussing race and ethnicity with patients. Revenue Cycle Coordinator Theresa Johnson, Care Navigation Program Coordinator Erica Ulibarri, and Patient Access Manager Kim Birrell led a pilot to test the list and develop practical learning for the system-wide implementation.
380 patients participated in the pilot at five locations spread throughout the organization, including the call center, or guest communications group. A pre- and post-pilot survey was conducted with 30 front desk and call center team members. We learned from the pilot that we needed to focus on small-group discussions with teams that explored the purpose of the project and how to build confidence in holding the conversations with patients. This helped refine our training program from a didactic one-way session to one more focused on conversation and learning together.
The pilot team helped to create learning materials for testing different ways of holding the conversation with patients. We found that providing a simple explanation of why we were collecting race and ethnicity information—to monitor and improve the quality of care—helped ease patients’ concerns, similar to the findings of a national study. These practical tools will support implementation and will continue to be refined as the project continues.
What’s next?
Beginning in late February, patients will now have a list of 77 combined races and ethnicities to choose from. These identities will map to existing Office of Management and Budget categories for submission to grants and reporting agencies.
It's an opportunity to talk about the importance of racial, ethnic and by way of relation–language diversity with our teams.
Leaders and front desk users will have opportunities for conversation and learning together, including how to sensitively ask for race and ethnicity and how to support each other as we learn and grow.
We’re starting to plan for the next phases of this project, including the sustainability of the racial and ethnic identity list. The list isn’t exhaustive, and we need a process to manage additions and subtractions. We aim to reduce our percentage of “unknown” or “other” in our patient population, and will evaluate for accuracy, timeliness, completion, and consistency.
We will stratify key performance indicators, such as quality and patient experience, by race and ethnicity. We’ve long operated under the assumption that if we treat everyone with the same quality of care, every person will have the same health outcomes. Soon, we’ll have data to show whether or not that's true. While we hope there are no health disparities, we know that they will be present due to historic and continuing systemic racism and marginalization. Soon we will be able to see more clearly where these disparities exist, and we can start to work together—community engagement, population health, and community partners—to create interventions that improve health outcomes for all.
RyLee Curtis
Sandi Gulbransen
Kimberly Killam
Mari Ransco
Michael Strong
Donna Baluchi
Huntsman radiation oncologist and population health scientist Gita Suneja, and maternal-fetal medicine specialist and racial, ethnic, and geographic disparities researcher Micelle Debbink, share five practical steps health sciences educators, researchers, and clinicians can take toward delivering more equitable care today.
Accurate, self-reported race and ethnicity data is necessary to create visibility of health disparities, provide inclusive care, and improve equity of health outcomes. Redwood Health Center’s Patient Relations Specialist Nichole Misner shares how to respectfully discuss this needed health information with patients.
Accurate, self-reported race and ethnicity data is necessary to create visibility of health disparities, provide inclusive care, and improve equity of health outcomes. Patient access manager Kim Birrell, Revenue Cycle Coordinator Theresa Johnson, and Care Navigation Program Coordinator Erica Ulibarri share tools for leaders to support employees.