The Value Equation of Answering Call Lights
Utah’s value equation is Value = Quality + Service/Cost. Improving response to call lights has elements on both sides of the ratio. A delay in response can lead to falls (quality) in the most serious situations. In every situation, wondering when someone will come to help erodes patient trust. Reducing call lights avoids the waste of nurses going back and forth to rooms multiple times. Value is improved by doing the right work, at the right time, when the patient needs it.
The Big Idea
By stepping back from the scores and focusing on reducing uncertainty and confusion, one inpatient nursing team piloted “purposeful rounding” to prevent patient-initiated calls, replacing the prior focus on improving the speed of response. The intervention achieved three outcomes: improved patient perception of responsiveness, increased patient safety and decreased nurse distraction.
The Challenge
ow fast is fast enough? Pushing the call button and waiting for someone to respond scares patients and interrupts caregivers. On average, a nursing unit can receive 7000 patient-initiated calls per month. At the University of Utah, a team on the Surgical Specialty and Transplant unit (SSTU) decided that rather than continually shaving seconds from the average response time, it was time to tackle the core problem. Could they help patients in real time, preventing the need for a patient to call?
The Plan
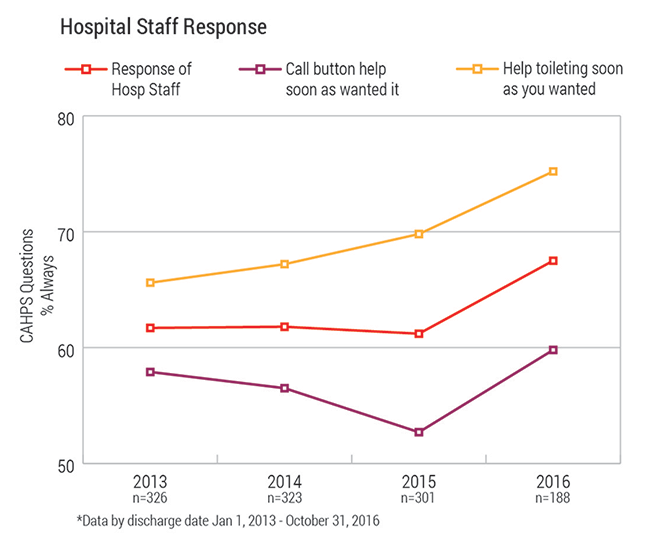
The nursing team on SSTU was frustrated by low scores on the HCAHPS surveys in the “Response to call” domain. This section encompasses two questions:
- How often did you get help toileting as soon as you needed it?
- How often did someone respond to you as soon as you needed it?
For many years, SSTU measured the time it took to answer a call light. Nurses and aids were fast, answering thousands of calls every month in under two minutes. They would drop what they were doing in order to answer a call light. Each month, publically posted graphs displayed each staff member and their average response to call. If the teams were so fast, why were patients still frustrated?
Meet the Team

Colline Prasad, RN

Kathy Schumann, RN
Colline Prasad, the nurse manager on SSTU, had a theory. As an experienced manager, Prasad knew what to do: ask patients. Prasad had led many changes that affected nursing practice over the years, and she knew that the best way to motivate staff was to bring the patient’s voice to the discussion. She listened to patients describe what it felt like to recover from a kidney transplant or bariatric surgery. Most patients had planned for months or years for their surgery, and were eager to get back to a “normal” life. They were used to being independent, so the thought of having to call for someone to help use the bathroom or to readjust their position in bed was frustrating, and sometimes embarrassing. Many patients think, “I’ll just try to do it myself.” Prasad discovered that when patients end up pushing the call button, it is after they have tried to do something and discover that they now needed help, usually immediately. Prasad understood that even though nurses and aids said, “If you need help, just call me,” every time they left the room, patients were reluctant to call until their needs were very urgent.
What if the nursing team tried to prevent patients from pressing the call button? If most patients have predictable needs, what if nurses and aids could try to meet those needs before they felt they had to press the call button? Prasad proposed her idea to two health care assistants (HCA). She asked them to keep track of how many calls they prevented during one shift and the strategies they used. It was already frustrating to run from room to room, never feeling like you could give a patient your full attention, so why not try something to lessen the demand?
The Strategies Used
1. At the start of the shift, after bedside shift report, go back into the patient's room and:
- Introduce yourself. Write your name on the white board.
- When you leave, tell them when you will be back, and then be back.
2. When you're in the room:
Try the new look, listen, and feel. Its not just for BLS anymore.
Look
- Make eye contact with your patient as much as possible. This is not only a sign of respect, but also a sign of confidence in your work.
- Are there signs in the room that the patient has emotional support? Are there flowers, pictures, or people? If a patient doesn’t have any of these items, the patient may need additional support from you by rounding more frequently.
Listen
- Is your patient an active participant or a spectator?
- Take a moment to give your patients your 100% attention. Take 90 seconds, make eye contact and listen.
Feel
- Be kind. You will never really know what they are going through.
- Many patients have a chronic illness. They are with us during an acute phase.
- Anxiety and anger are usually a side effects of fear.
3. When You're in the room, look at or ask about...
- Water: Has to have ice or marked no ice
- Phone: In reach and charged
- Food
- Alarms: IV bags with at least 200 in them at all times, pumps plugged in.
- Bathroom
4. Round before you go on break and right before you finish for the day.
5. If you're busy, ask for help. This is a skill everyone has and everyone can do.
6. Avoid saying: "Turn on the call light if you need anything." Instead, say: "I'll be back in about one hour. Try and get some rest."
7. If a call light does go off, it's 911, all hands on deck.
Improvement principle used: Correct vs. Prevent
Often, we design an intervention to prevent a problem from happening again. In this case, the patient thinks we take too long to respond to the call light so we work harder to respond faster. That effort did not result in the expected change – happier patients. At times it had a negative consequence – more scattered nurses.
Safety thinking is focused on preventing the problem from happening in the first place. After repeated cycles focused on correction, Prasad and team redefined the goal – prevent the calls in the first place. With the shift in problem definition, the team was able to unlock new options with dramatic results.
The Metrics
Reflection
Prasad and the nursing team were surprised that many patient calls can be prevented, and those patients believed they were getting better care. The team has decided that they will implement “purposeful rounding” in the entire unit. They will continue to track time to respond to call, but they will also begin to track the number of calls received every month. Prasad reflected that “it feels counterintuitive to round before you complete major tasks with patients and many don’t see it as a way to save time. But, its actually a way to save time and keep patients safer.” The team can be proactive, instead of reactive. The process of listening to patients has been a powerful ongoing motivator for staff.
Think this might work for you? If so, Kathy Schumann's SlideShare will be helpful:
Mari Ransco
Chrissy Daniels
Steve Johnson
Kathy Schumann
Colline Prasad
University of Utah Health’s success is driven by teams doing the right work for our patients — and sharing that work across the system. Chief Medical Quality Officer Bob Pendleton reflects on the universal importance of continuous improvement while looking at health care through the eyes of a patient.
Waiting is such a firmly entrenched feature of healthcare that it is often taken as a given and not recognized for the disrespect it conveys.
Many people ask, “What am I supposed to report?” or “Does this count?” Hospitalist Ryan Murphy explains the basic vocabulary of patient safety event reporting, informing the way we recognize harm and identify and report threats to safety.