Learning Objectives
After completing this lesson, you will be able to:
(1) define quality improvement
(2) explain when you should and should not use a QI approach
(3) List two concrete steps you can take to get started with your QI project.
Download Slides: PPT
Case Study
Continuous electronic monitoring with telemetry is an important hospital practice for monitoring patients who are at high risk of serious cardiac events. Unfortunately, it is often overutilized. When hospitalist Karli Edholm learned that 25% to 35% of patients on her service were being monitored on telemetry—most unnecessarily—she was annoyed. For years, she educated physician trainees and discussed criteria for appropriate use, but she saw little effect. Tired of the inertia, she decided to change course. She worked with an interdisciplinary team to introduce a bundle of interventions, including education, audit and feedback, financial incentives, and changes to electronic orders. Her efforts reduced telemetry usage to less than 10% without any evidence of harm to her patients.
What is quality improvement?
The Department of Health and Human Services defines quality improvement (QI) as “systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups.” Within this definition, three words should be emphasized. The systematic approach of QI helps create effective interventions that lead to sustainable improvement without leading to adverse effects elsewhere in the system. The continuous nature of QI recognizes that the work is never done and embraces the merits of constant improvement. Lastly, the emphasis on measurement in QI ensures that actions taken lead to demonstrable change for the better.
Background
Quality improvement as a concept rose to prominence in the mid- and late-20th century as part of a shift in manufacturing management philosophy that focused on improving product quality while reducing production costs. The concept reached national prominence in health care in the early 2000s following the release of two landmark reports from the National Academy of Medicine (To Err is Human and Crossing the Quality Chasm). The reports highlighted the gap between what we define as high-quality care and what patients actually experience, providing a call-to-action around health system redesign.
As in manufacturing, quality improvement in health care is one part of a larger strategy around leadership, management, and policy reform. For the purposes of this series, we will focus specifically on quality improvement as an approach to local improvement.
Methods
In health care, we often have little trouble identifying outcomes we wish to improve—patient falls, medication errors, readmissions, etc.—but struggle to implement effective, sustainable solutions. Often, the problems we face are complex, and are not easily addressed with simple interventions. Or interventions that we previously deployed fail. Structured quality improvement approaches—or improvement methods—provide processes and tools for measuring and managing your efforts in a way that helps sustain improvements in your local environment.
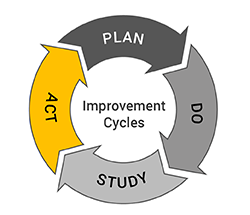
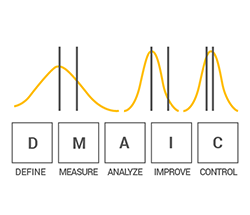
You may have heard of different models for quality improvement, like Lean, DMAIC, or the Model for Improvement/PDSA cycle.
| PDSA | LEAN | SIX SIGMA | DMAIC |
|---|---|---|
 |
 |
 |
| What it is: Plan-Do-Study-Act (PDSA) is a cyclical approach that supports small tests of a change. | What it is: Lean focuses on systematically eliminating waste in every process, procedure, and task. | What it is: Six Sigma systematically decreases variation in processes to achieve a consistent outcome. |
| When to use: This is the most commonly used approach to improvement. Great to use for first-time improvers and low-stakes problems, but insufficient with increased complexity. | When to use: Identifies Seven Wastes and is full of helpful process tools. Karli’s telemetry overutilization project is an example of eliminating waste (unnecessary testing). |
When to use: Define, Measure, Analyze, Improve and Control (DMAIC) is Six Sigma's data-driven strategy for improving processes. Typically for high-stakes, high complexity projects. |
At the University of Utah, we use the Value Framework, which incorporates principles from all of these models. The use of a systematic approach is more important than the particular method you use.
When to use quality improvement
Quality improvement excels when one is faced with complex problems, but it is not appropriate in all situations.
Below are three common improvement scenarios you will encounter in the health care setting.
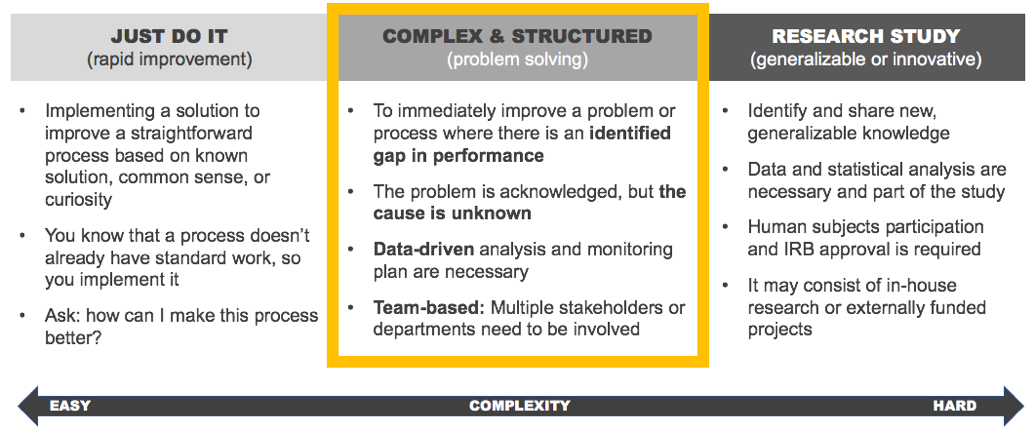
Use it to solve complex problems
Complex problems (👍): In our case example above, Karli identified a problem—overutilization of telemetry—but initially struggled to find a solution. As a physician educator, she naturally turned to education, but found it was minimally effective and unsustainable without continuous effort on her part. Solving the telemetry problem required collaboration among her peers, residents, nursing, data analysts, and others to sustain. Truly a complex problem with no easy solution.
Don't use it to solve simple or research problems
Simple problems (👎): Karli had to use a systematic approach because the problem of overutilization of telemetry was complex and failed to improve with simple solutions. If only a few providers were ordering telemetry inappropriately, her initial approach of education alone might have proved sufficient. Any quality improvement effort will require an investment of time and resources. Save that investment for those problems that are important to you and your organization and are complex enough to require a collaborative, longitudinal commitment to develop interventions that stick.
Research problems (👎): Telemetry overutilization is a well-known phenomenon, and Karli could point to well-established guidelines regarding appropriate use. Rather than discovering new knowledge, she brought existing knowledge into practice to improve care for her patients. Quality improvement is not the same as research, and differentiating between the two can be confusing.
If your primary intent is to contribute to generalized knowledge, a research approach may be more appropriate. If your primary intent is to improve delivery of care or health outcomes for a local population, a quality improvement approach may be right.
More information on the difference between improvement and research here.
How to get started
If you’re thinking about leading or participating in a quality improvement effort, here are three concrete steps to get started:
1. Continue your independent learning
- Explore other lessons on Accelerate
- Take the Value Improvement Leaders course (internal resource)
- Explore external resources (like IHI Open School)
2. Find a mentor or coach
- Talk to your manager, program director, and/or colleagues to learn about mentors, projects, training, and other opportunities unique to your area
- Contact U of U Health’s Value Engineering for information on their coaching methods (internal resource)
3. Have a plan
- Try using the Project Readiness Assessment, a 13-question guide to help think through your project
Conclusion
When used effectively, quality improvement can create lasting and meaningful change for patients, families, and those who work in health care. It’s empowering to have the knowledge, skill and ability to make care better. Learn how and when to drive improvement in your local health care environment.
Originally published January 2019
Ryan Murphy
Improvement science is about making everyday tasks easier and faster. This week, Steve uses the 6-phase value improvement methodology to build a highly-reliable morning routine.
This week, Steve describes a genius (yet simple) data collection tool: the check sheet. Colline Prasad and the SSTU nursing team used check sheets in their work reducing call lights, a project that turned out to be a triple-win; an intervention that improved patient perception of responsiveness, increased patient safety, and decreased nurse distraction.
If Apple Maps and Garmin can provide just-in-time information, why can’t health care? Lots of legitimate reasons, but we’re making significant strides. This week, the Dojo goes moto as Ken Kawamoto, Associate Chief Medical Information Officer and Director of Knowledge Management and Mobilization, helps us understand how we’re creating better information at the right time.