ncreasing access to primary care is vital to improving healthcare in Utah and across the country. During the pandemic, with the expansion of virtual visits, University of Utah clinics faced a particularly challenging access problem: patients could schedule an in-person visit via the MyChart patient portal, but they were required to call to schedule a virtual visit.
For many common problems, virtual visits make seeing your primary care provider easier. Virtual visits help patients overcome many access issues like transportation challenges, busy schedules, and mobility issues. They also save patients money. When there’s no need to travel to a clinic, travel expenses are zero, and many patients avoid child care expenses and lost wages from missed work. Our team needed to make it easy for those who would benefit from a virtual visit to get one, while guiding other patients to the office when that was more appropriate for their care.
Designing a new way to self-schedule appointments
Together, our team created a pilot where patients were given access to a new process for scheduling virtual appointments at Madsen Family Practice. We chose this practice for the pilot because it has high MyChart utilization among patients and providers were very eager to offer patients self-scheduling. One of our key challenges during the development of this self-scheduling tool was that we needed a system that would effectively and efficiently guide patients to the appropriate visit type: virtual or in-person. With so many variables—what can and cannot be done well in a virtual visit, patient demographics, lab work and other needs—this was quite a challenge.
Our team developed a decision tree that carefully guided patients to the best place for care, given their reason for visit and other factors. The goal of this decision tree was to limit the number of questions for patients so that the process would not be an additional barrier to access. Fortunately, we were able to place this decision tree within the MyChart platform and use intrinsic data available like patient names, ages, and pre-existing conditions to streamline the number of questions. The integration of scheduling into MyChart helped create important efficiency for this process.
Development of the self-scheduling platform
The team had to carefully choose who could self-schedule a virtual appointment and who could not using a decision-tree integrated into the MyChart platform. It took two months of teamwork, communication, and testing just to get these questions refined before the pilot began. This is a general list of concepts that were refined during development of the decision-tree.
-
Safe care – The patient is first screened for physical and psychological safety. Patients with life-threatening symptoms are directed to use 911 or to access their nearest emergency room.
-
Appropriate care – Patients are given a list of concerns that are not appropriate for virtual care and guided away from virtual visits if they had concerns on this list.
-
Effective care - Patients are asked if they need labs, immunizations or imaging of any kind. These patients are guided to an in-person visit.
Outcomes of Mychart virtual visit self-scheduling pilot
After five months of this pilot, the team saw clear benefits to self-scheduling. Prior to this pilot, there were several concerns about using an automated scheduling platform. The first concern was that patients would not be able to safely and effectively determine when a virtual visit is appropriate. Additionally, an ineffective process would lead to additional work for the clinical teams. Data from the pilot, however, showed that patients, given appropriate guidance in the scheduling platform, chose a virtual visit only when it was appropriate for their care. That is, once a visit was scheduled via the decision tree, visit types were rarely changed by clinic staff; providers were comfortable with patient selections.
The second concern was that virtual visit self-scheduling would increase the overall number of virtual visits dramatically. Data from the pilot showed, however, that the rate of virtual visit and in-person visits were fairly constant before and after self-scheduling was enabled.
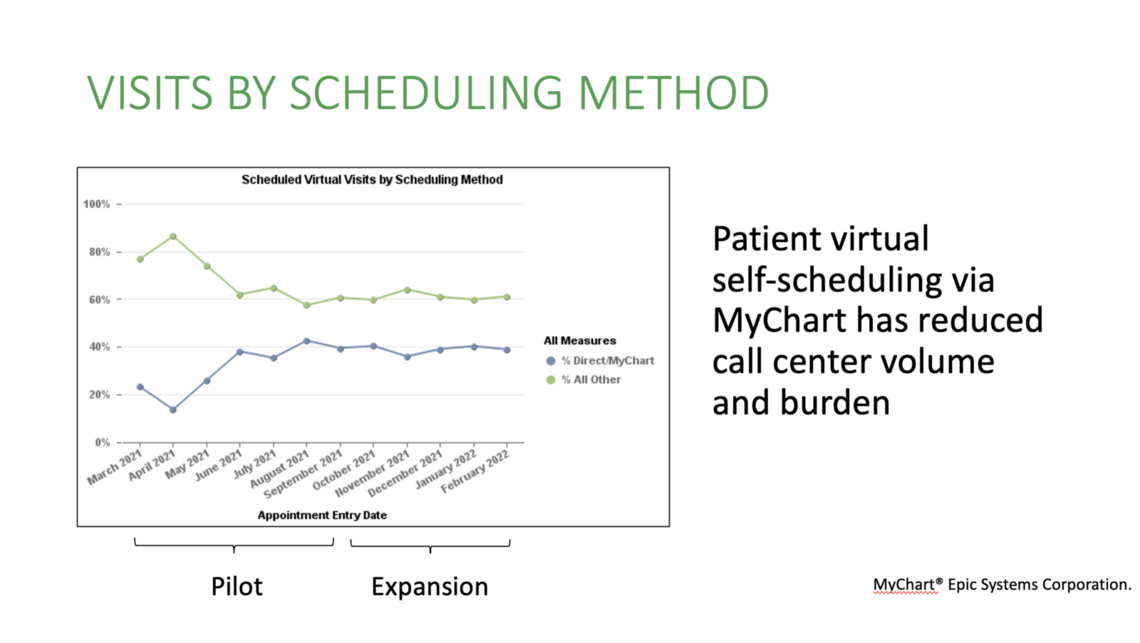
Data from the pilot showed integrating this automated process did not create extra work for our clinical teams. It also showed clear benefit to the system as a whole. Virtual visit self-scheduling is more efficient and results in high patient satisfaction. It is also more cost-efficient. Each time a patient schedules a virtual visit through the MyChart platform, instead of using the call center, the process is less costly for us as a health system. Because there is labor involved in having a call center employee safely and efficiently navigate a list of screening questions, virtual visit self-scheduling saves approximately $3.50 per visit scheduled.
Data from the virtual visit self-scheduling pilot showed that patients who accessed the platform had high satisfaction with the process. The clinic as a whole also maintained a high level of patient satisfaction for both in-person and virtual visits.
This follows the general trend that improved access to care is a key part of patient satisfaction.
Quality and patient satisfaction was measured during the pilot. Data showed that patients were screened for depression, a common quality metric, at a higher rate during completed virtual visits. Interestingly, we did not see higher patient satisfaction feedback on the ease of scheduling during the pilot, but we did see higher patient satisfaction with their care provider.
Expanding access to self-scheduling
With such great data from the pilot at Madsen Family Practice, we were able to expand virtual visit self-scheduling to the practices in the Community Physicians Group, as well as two other practices in the Department of Family and Preventive Medicine. The Behavioral Health team has also begun using this scheduling model in their practices and other specialties are exploring this option.
We are incredibly proud of our outcomes and the interest in our project. With such strong data, we feel confident that virtual visit self-scheduling can benefit many practices within the health system, making it easier for patients to get the care they need, improving the scheduling experience and convenience, reducing cost of scheduling, and maintaining excellent patient experience and quality of care.
Susan Pohl
Lindsey Garcia
Bernadette Kiraly
Erin McCormack
Health care delivery is ripe for digital disruption. How are we preparing for the future at U of U Health? Chief Information Officer Donna Roach outlines the path forward and what it takes to transform health care to meet an increasingly digital future.
Expert communicators Emily Izzo and Bridgette Maitre share how to ask open-ended questions to encourage conversation and promote meaningful connection.
University of Utah Health’s director of patient experience Mari Ransco examines the pandemic patient experience through the lens of the 5 Elements: U of U Health’s qualitative model for delivering an exceptional patient experience.
