hink about the last time you or a family member went to the doctor. Was it easy to make the appointment? How was the experience once you were there? Did you feel safe and heard? Did you have to get a test, like an MRI or a blood draw? Or pick up a prescription? Did all the steps feel coordinated and easy? How about paying your bill?
The experience of health care stands out among our experiences as a consumer. Shopping in health care isn’t the same as shopping for a commodity, like a car, or the service you get when ordering a cup of coffee. There aren't a wide variety of understandable choices at multiple price points.
In health care, we are both patients and consumers. Learning this distinction can help us further our commitment to patient-centered care. It’s a natural extension of our promise to deliver an exceptional patient experience.
Commoditization misses the mark
I am increasingly in conversations where someone relates health care to another service industry. At national conferences, consumer decision-making in health care is met with a collective shudder as we consider other industries entering our market.
But talking about consumerism in health care this way misses something central: the vulnerability we feel when we’re a patient. The worry and anxiety we feel as a family member.
The stakes are higher in health care. The mission, people’s “why,” is what motivates people to work here, to continue to show up after a bad day, to be present with someone in their time of need, to solve their problem, to care and to comfort. Reducing this kind of care to “consumerism” can feel like cheapening the work.
"Talking about consumerism in health care this way misses something central: the vulnerability we feel when we’re a patient. The worry and anxiety we feel as a family member."
There is another important distinction: unlike the pilot, mechanic or barista, we are all patients and family members. When we work in health care, we are both the givers and receivers of our services. This fact introduces the potential for tremendous competitive advantage. When we harness this experiential knowledge, we can design care processes that meet our patients’ needs in ways other industries cannot.
Distinguishing between “patient” and “consumer” needs
I have found it helpful to distinguish between when to focus on meeting patient versus consumer needs.
Patient needs
We are patients when we are in the room, on the exam table, or in the patient bed. In this moment, we are vulnerable and at the mercy of our caregivers. We expect respect and acknowledgement of this vulnerability. We make decisions based on how much we trust the team. We want to be listened to, cared for, and treated like we matter. We want the team to be empathetic and to understand the physical and emotional tolls of illness and injury.
Questions to address patient needs:
- Are we listening with intent?
- How are we helping our teams to be more emotionally present when it matters?
- Do we have a clear vision of how we want patients to perceive us? Is that vision shared by the team?
Consumer needs
And yet we’re consumers at the very same time. We expect that our information is shared between our doctors and that they're working together to deliver our care. We want it to be as easy as possible with the fewest calls or clicks online to make an appointment. We want timely and clear follow-up from tests, results, and next steps. We want the system to value and respect our time. We demand that our personal information is protected and private. We want to know that the clinician has considered the cost of care.
We want it to be easy, using the tools that we’re used to in other parts of our lives—the ability to schedule online, easily accessible information, and seamless follow-up with prescriptions and bills.
There is a tendency to conflate “consumerism” in health care with making health care more convenient. And it's true, health care does need to become more convenient, especially for healthy patients. But consumerism also means that we consider patients not just the passive recipients of our care, but as actors with agency and choice. It means that we must listen and respond to their priorities.
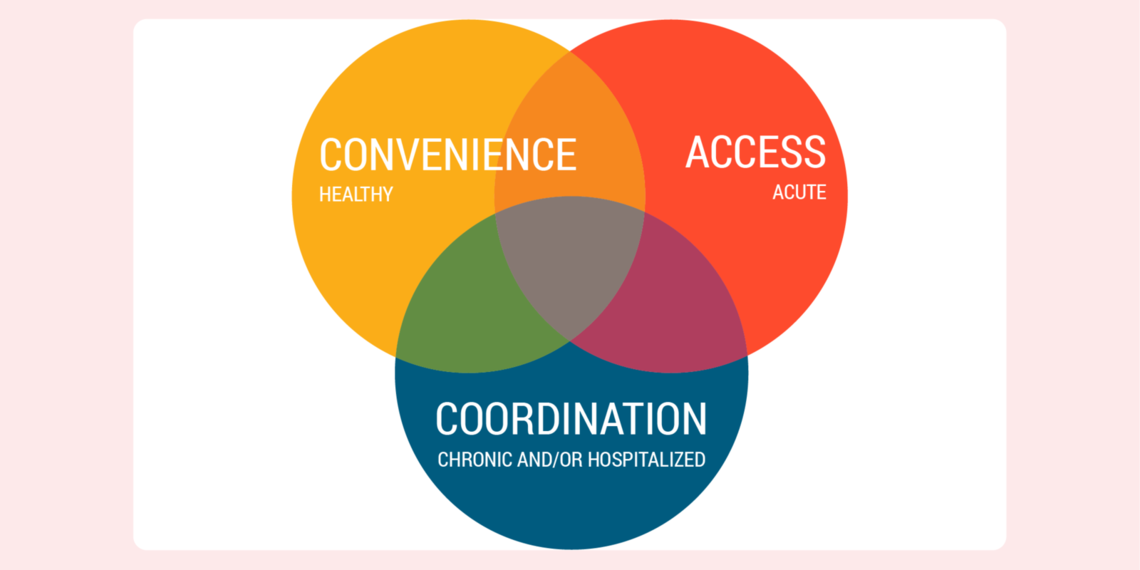
"When patients are healthy, convenience is prioritized. When a patient is chronically ill or hospitalized, coordination steps to the forefront. When a patient is acutely ill or injured, access is most important."
Those priorities broadly change depending on health status. Qualitative analysis of thousands of patient comments reveal that when patients are healthy, convenience is prioritized. When a patient is chronically ill or hospitalized, coordination steps to the forefront. When a patient is acutely ill or injured, just being seen—access—is most important.
Questions to address consumer needs:
- What are we doing to understand and improve unnecessary delays?
- How’s our wait time? Should we examine our template?
- Do we have consistent processes for everyday activities (such as bedside shift report or myChart messages)?
Harnessing the power of both
When care is communicated as a commodity, it feels disempowering. However, like most things in life it’s not that simple: we are all patients and consumers, at the same time. We all want and need the same things.
Understanding this distinction can help us further our commitment to patient-centered care. It’s a natural extension of our promise to deliver an exceptional patient experience.
The Power of Patient Voice
We asked Rusty Andrade, a member of U of U Health's Patient Design Studio, to weigh-in with his thoughts on the changing patient experience as a patient and employer in this state.
"In most industries, the primary goal is to find the most efficient way to deliver products and services to the consumer. The latest smartphones, the best quality clothing or the most delicious ice cream are provided with convenience and profit in-mind.
What about the consumer of health care products and services? The growing role of the patient as a consumer is pushing providers and clinics to think critically about the way they can create positive experiences for their own consumers.
In 2020, the cost of insurance is estimated to increase more than 5% in most U.S. markets with the average family plans costing $15,375 according to the National Business Group on health. When combined with high-deductible out of pocket costs, the average Utahn could anticipate spending as much as 23% of their annual income on health care. When investing these resources, often during times of increased stress and pressure, the patient voice in the health care journey is more important than ever."
—Rusty Andrade, JD, Patient Designer, U of U Health Patient Design Studio
Mari Ransco
University of Utah Health’s director of patient experience Mari Ransco examines the pandemic patient experience through the lens of the 5 Elements: U of U Health’s qualitative model for delivering an exceptional patient experience.
Patient Experience Program Coordinator Corrie Harris and Project Administrator Shayma Salih explain how to get valuable patient feedback early in your improvement efforts by meeting with the U of U Health Patient Design Studio and Advise Utah.
Palliative care teams focus on treating the symptoms and stress of serious illness. Nate Wanner, Associate Medical Director of U of U Health’s Palliative Care Program, discusses how palliative care not only improves the quality of a patient’s life, but supports other clinical teams in one of the most challenging (and rewarding) parts of caring for people: having hard conversations.