
Around 140 surgeries and other invasive procedures take place in our hospital system each week day—and at each one, a surgeon will walk into the operating room and find his or her instruments waiting. For surgeons, sterile instruments are like electricity or any other utility; a lean system is out there delivering what’s needed, where and when it’s needed, while remaining out of sight and out of mind.
This video and process map highlights the professionals of Sterile Processing as the stewards of our surgical instruments. An integral part of the system required to provide safe and efficient surgery, sterile processing is a much larger and more sophisticated operation than most understand.
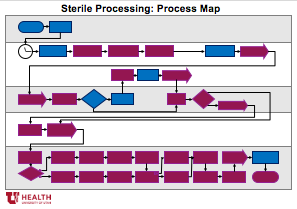
Sterile Processing: View the Process Map
Lean Practices in Action
Sterile Processing’s lean operation employs a series of lean practices defined below.
1. Forcing functions
Forcing functions help us do the right thing for patients while reducing the cognitive load. A forcing function is a control in the process designed to prevent errors. Some forcing functions are process steps requiring conscious consideration of the process (e.g. an OR time-out) while some are error-prevention mechanisms (e.g. a three-prong plug).
2. Doctor Preference Cards (Checklists)
A common forcing function to prevent the error of missing a step or, in this case, an item. Simple in concept but requiring multiple iterations to develop and discipline to use.
3. Barcodes
Another common forcing function to reduce the errors associated with more manual inventory tracking methods. Barcode scanning is fast, reliable, precise, and provides immediate feedback — “beep” is good, “bong” is bad.
4. Layout (as forcing function)
Lean layouts are often agile, allowing adaptation to changing requirements. Indeed, much of Sterile Processing’s equipment is on wheels for this purpose. However, SP’s segregated layout ensures against contamination: instruments flow in a single direction from the dirty zone to the clean zone to the sterile zone.
5. Just in time (JIT)
Getting the right material and equipment into the right hands, at the right time, defect-free.
6. The waste of travel
Traveling from place to place doesn’t add value to the service we’re providing. Whether it’s the patient, staff, stuff, or information, travel should be minimized.
7. Quality control mechanisms
These mechanisms offer hard evidence that vital quality thresholds were met. For example, the required temperature was reached, or bacteria died. Quality control mechanisms tell us whether an error occurred after the process step; forcing functions prevent the error from occurring in the first place.
More Lean Behind the Scenes:
Follow Utah’s Nutrition Care Services as they produce and deliver over 300 lunches to inpatients all over our hospital, all at the same time.
Credits
Special thanks to Janet Paschal and the entire Sterile Processing team for sharing their time and expertise to make this video possible, along with the combined creative talents of Charlie Ehlert (Steadicam videography, special effects, and video editing) and Jen Pilgreen (time-laps and GoPro videography).
39th Annual Telly Award Winner Package: University of Utah Health "Lean Behind the Scenes: Sterile Processing" - 2018 Telly Awards Bronze . Category: General-Employee Communications for Non-Broadcast.
Steve Johnson
Visual cues in the workflow reduce cognitive load and help process stakeholders make the right decision. Steve Johnson interviews Dan Vargo in this Lean Behind the Scenes exclusive.
Hospitalist Ryan Murphy introduces quality improvement (QI): The systematic and continuous approach to improvement.
Thinking about teams differently did more than improve our inpatient discharge process. It gave everyone a shared vision: every single patient in the right bed, at the right time. Patients now leave the hospital earlier, all while monthly discharges have increased. Tracey Nixon, director of capacity management, shares how they did it.
